Infrastructure related issues-
Due to focused efforts by the government, there has been an improvement in the basic health system infrastructure. Number of sub-centers, Primary health centers (PHCs) and Community Health centers (CHCs) have increased over the last decade and serving somewhat in the recommended range of population that each should be serving. However, there are specific areas of improvement to make them functional as per norms set by the government (Indian Public Health Standards-IPHS).
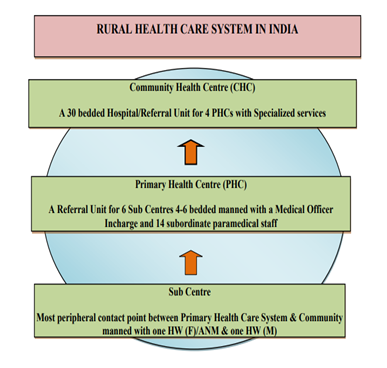
This is the basic framework of rural healthcare system in India. There are minimum staffing recommendations for each with tribal/hilly areas having denser requirements.
The tribal villages, especially those located in highlands are sparsely populated and the houses are spread over a vast area makes it challenging to provide essential primary healthcare to the inhabitants.
State-wise data* also suggests that in Chhattisgarh, each sub-center, PHC, and CHC cover a greater amount of distance as compared to national average, (e.g. average area covered by a sub-center in Chhattisgarh is 25.35 km2 while same at national level is 18.98 km2) highlighting the issue of accessibility and importance of connectivity by motor-approachable road and availability of affordable/free transport services.

Visit to one such village having a stone covered path for 2-2.5 km connecting it to the last traces of a road brought into limelight the problem of inaccessibility. In an emergency, if the ambulance fails to reach due to multiple operational issues, people are forced to carry a pregnant woman on a cot lifted by 4 people or worse in a ‘mitti-uthanewala’ sling (a kind of a beam balance to carry humans-as depicted in the photograph). And when asked what if there are no men around, a pin-drop silence pitched in. The pain in their eyes gave them away. Also, in Surajpur, which was part of Surguja until very recently, 78 villages get cut-off from the district roads due to rains. Sixty-nine such villages belong to a single block, Odgi, home to the most disadvantaged populations of Pandu and Pahadi Korwa tribes.
Manpower related issues-
There is stark shortage in healthcare staff that is quite evident from information from (sources) This remains true even at the district level. Due to no full-time anesthesiologist at a district hospital in Chhattisgarh for 8-9 months, patients had to be referred to another district for even a caesarian section. This has become a norm rather than an isolated state of events. It has been a challenge to attract and retain trained/specialist medical personnel in rural areas.
We found a similar scenario in our visits to district hospitals, community health centers, primary health centers and sub-centers of Surguja and Surajpur where specialists were present mostly in the district hospital and that too in limited numbers. MBBS medical officers mostly manned the community health centers and Assistant medical officers (AMOs- a separate cadre of health workers trained in a course of allopathic medicine to cater to primary care needs of rural areas for 3 years in Chhattisgarh) were in charge of most primary health centers.
Summary
We find the situation in Surguja a reflection and a complex intersect of chronic neglect and deprivation of the indigenous communities in terms of opportunities related to employment, education, administrative and political space, systemic underfunding of systems needed to address such asymmetry in opportunities and geographic and topological challenges of the area.
This has resulted in the region lagging behind in terms of social determinants of health and the resultant poor health outcomes. The practices of inter tribe discrimination (not as rigid as caste discrimination but still prevalent) and the social condition of women in the community (similar to other parts of the country) adds to the complexity.
The health outcomes reflect some of these realities in the form of poor indicators for maternal and child health and problems common in tropics like snake bite, malaria and tuberculosis. The rising burden of non-communicable diseases consistent with other parts of the country adds to the disease burden.
The health system challenges in the form of poor infrastructure and manpower shortages aggravate the disease burden further. It also erodes the trust in public health system diverting people to private sector thereby increasing their out of pocket expenditure. The poor health outcomes and increasing expenditure on health only add to the state of chronic deprivation in the area.
Going forward to get a better understanding of the context of our area of work and its complexities and to foster a bond of love, care, trust and mutual respect, we would need to spend more time with the communities we work with.
*Government of India Ministry of Health and Family Welfare Statistics Division. Rural Health Statistics: 2018-19. Delhi, December 2019. Available from: https://main.mohfw.gov.in/sites/default/files/Final%20RHS%202018-19_0.pdf
